DEVELOPMENT AND EVALUATION OF POLYHERBAL DERMAL FORMULATION
HTML Full TextDEVELOPMENT AND EVALUATION OF POLYHERBAL DERMAL FORMULATION
Vishal H. Thorat *, Sachin S. Ghorpade and Tushar Patole
Department of Pharmacognosy and Phytochemistry, SGB Amravati University, Amravati - 444604, Maharashtra, India.
ABSTRACT: The plants are used to treat skin infection as well as cuts, burn, dermatophytes and infectious disease are common in traditional medicine. The development of new polyherbal dermal formulation treat against resistant pathogens is increasing interest. Therefore, the aqueous, methanolic extracts from different parts of four medicinal plants used locally in folk medicine were evaluated for wound healing, antimicrobial activity. Different types of aqueous plant extract potential to treat cuts, wounds, fungal infection without any adverse effect of plant extract. It was found that most plant extracts studied had antibacterial and antifungal activities. The extract showed significant activity against all tested bacteria and showed higher antifungal activity against E. coli.
| Keywords: |
Wound, Formulation, Evaluation Parameters
INTRODUCTION: Herbal Medicines: Four billion people or about 80% of the world's population uses herbal medicine today as part of health care. Different cultures use herbs located in their geographical locations for curing common illnesses. They have been successful to a certain extent and over many centuries, some of the herbal cures have proved to be far more useful than allopathic drugs. What exactly is herbal medicine? One can loosely describe it is a natural form of healing or alternative therapy where herbs and plants are used in the form of extracts, pills, syrup or powder to cure ailments or diseases of human beings and in some cases of animals too. The administration of herbal medicines has been on a profile until now.
But the failure of some allopathic drugs and its side effects have prompted some patients to go back to ancient healing methods which use herbal medicines to give relief 1. Herbal medicines are also called as herbalism. Ancient Chinese, Indians and Europeans discovered the origins of medicinal herbs. They have been using them for curative purposes successfully. The records are available in ancient texts. In India itself, there are more than 1100 medicinal plants grown all over the wild forests.
Of these, some 60 genuses are used immensely in medicinal preparations. Despite their demands today, they are not grown in a controlled manner. Rather tribes use them as their livelihood in some belts where they are grown in the wild. Unlike India, in China, the spurt in demand for traditional medicines has made the government allow the growth of these plants for further research and development. About 100 units have nearly 600 plant types, grown for their medicinal value. Herbal medicines are used in Ayurveda, Naturopathy, and Homeopathy, traditional and Native American medicines. About 74 plant types are used in modem medicines. They are bought from rainforests 2. With due importance, healthcare is being given worldwide; it is strange that herbal medicines are being used quietly without the consultations of a practitioner. They are bought over the counter or from unqualified people who make them as they hardly have, any side effects patent medicines are few in circulation, especially in India and China. In general physicians and doctors combine them with allopathic drugs for patients with chronic problems, it could be a positive step towards healthcare. As they are cost-effective, they fall within the budget of patients needing long-term care.
Role of Herbal Medicine: If we discount allopathic drugs as the most preferred method of getting the cure, then we safely say without any side effects that alternative herbal medicine is gaining more popularity. If properly guided it can turn into a billion dollar industry for Indians and Chinese who grown these medicinal plants. Traditional methods of curing ailments through botanical herbs and medicinal plants have become trendy. Many patients who are not happy with prolonged drug treatments are rooting for alternative healing therapy. As herbal medicines are becoming a trend for the latest healthcare all over the world, it is better to understand the basics, which have been lost in antiquity 3. Primitive residents of the ancient world experimented on a trial and error basis to cure painful toothaches, bruises, and wounds. They used leaves, barks, and saps (oils). It worked sometimes, and at times, it failed. Some continued research and developed their skills to recognize the medicinal qualities of certain valuable plants. As civilizations improved so did their methods of curing themselves.
From local anaesthesia to surgeries, plain dressing of wounds, common colds cough and fever variety of plants was used. These medicines worked along with faith and prayers (not common in modern medicines), and surprisingly they created miracles! Most of them worked well because they went deep down to the root cause of the disease. They worked slowly to stem the rot and were successful experiments. Today the world recognizes three types of traditional methods of herbal medicines going by various case histories of treatments over the centuries 4.
The western world depends largely on Greek, Roman and other medieval sources of alternative healing. In the East, India offers Ayurvedic solutions of many types. Chinese herbal medicines also have a large following with its rich history. What has been a common factor for all these three types is that none of them worked on any scientific principles. A combination of faith and common knowledge helped general physicians to cure their patients. They tackled the root cause of the problem rather than look at the effect. Time and skill helped some to identify herbs and plants.
Ancient Chinese discovered 2,000 such plants. Some had curable effects; some were sheer poison and fatal. Generations of Indians and Chinese tell tales of miracles and recoveries due to some 'jadi-booti'. It is very strange that modern scientists are still not acknowledging the use of these medicinal plants. For them 'what is herbal medicine' except an unqualified dose which may or may not prove to be successful. The fact that some of the allopathic medicines do use plant extracts is helping in changing scientific minds. Embracing the ancient methods would be far more useful and lucrative instead of shunning its historical value. Introducing traditional medicinal courses in colleges would help the young generation of doctors to improve their knowledge and hone skills. Having a holistic approach to herbal medicines and its cures is a sure shot prescription for new practitioners 5.
Indian Herbal Medicine: Much of ancient India's contribution to the medicinal world is surrounded in myth, legend, and superstition. Especially when it comes to traditional methods of cure, the west has looked the way suspiciously; it works without any scientific reasoning. However, the truth lies out there in millions of people worldwide now turning to ancient Indian sciences to take care of their health. Whether it is yoga, Ayurveda, Homeopathy or any other form of naturopathy, there are enough people wanting to try out alternate ways of healing. With celebrities endorsing some of the forms, they have become popular. Indian herbal medicines use various herbs and roots, sometimes succulents, different mushrooms, cacti, and seeds. Some of these herbs have been used to correct cosmetic problems like acne, skin ailments, making perfumes also.
Indian spices used in the kitchen until today are useful, and generations of Indians depend upon them for their curative properties. Unani doctors, Ayurvedic, prescribe them and Homeopathic doctors respected for their skills in weeding out the root cause of many diseases. Even diabetes, depression and other modern-day diseases are tackled or controlled with the correct use of these medicines. Some of the ingredients are used as nutritional supplements, and local companies make popular health foods and drink supplements with the trend falling back on remedies of the ancient world, various myths are being busted and proper reports are being released to help people to decide what remedies are suitable to them 6.
This is a positive sign for the Indian herbal medicine industry as it capable of turning into a profitable venture for local pharmacies that have been producing products of medicinal value for more than half a century or more than that. The government of India also felt the need to support the ancient health systems and in 1995 established 'Indian Systems of Medicine and Homeopathy' (ISM & H) now known as Ayush (Ayurveda, Yoga, Unani, Siddha, and Homoeopathy). With recognized courses in training and teaching institutes, it is a step forward to allow practitioners of alternative healing therapies to work alongside allopathic doctors on par. This will reduce the problems of quacks also. Proper funding for research and development will also allow ions to conduct tests and improve on the medicinal systems already existing. As they are cost-effective and been used for long, it will help in exploring and curing many ailments.
Skin diseases are among the most common health problems worldwide and are associated with a considerable burden. The burden of skin disease is a multidimensional concept that encompasses psychological, social and financial consequences of the skin disease on the patients, their families and on society. Chronic and incurable skin diseases, such as psoriasis and eczema, are associated with significant morbidity in the form of physical discomfort and impairment of patients' quality of life; whereas malignant diseases, such as malignant melanoma, carry substantial mortality. With the availability of a wide range of health status and quality-of-life measures, the effects of most skin diseases on patients' lives can be measured efficiently. This review aims to present some of the published data to highlight the magnitude of the burden associated with some common skin diseases and also to suggest ways to quantify this burden of skin disease 7.
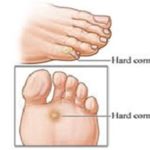
An ear of corn (or clavus, plural clavi or clavuses) is a distinctively shaped callus of dead skin that usually occurs on thin or glabrous (hairless and smooth) skin surfaces, especially on the dorsal surface of toes or fingers. They can sometimes occur on the thicker palmar or plantar skin surfaces. Corns form when the pressure point against the skin traces an elliptical or semi-elliptical path during the rubbing motion, the center of which is at the point of pressure, gradually widening. If there is constant stimulation of the tissue producing the corns, even after the corn is surgically removed, the skin may continue to grow as a corn 8.
Presentations: The hard part at the center of the corn resembles a barley seed that is like a funnel with a broad raised top and a pointed bottom. Because of their shape, corns intensify the pressure at the tip and can cause deep tissue damage and ulceration 1. Hard corns are especially problematic for people with insensitive skin due to diabetes etc. The scientific name for a corn is heloma (plural helomata). A hard corn is called a heloma durum, while a soft corn is called a heloma molle. The location of soft corns tends to differ from that of hard corns. Hard corns occur on dry, flat surfaces of skin. Soft corns (frequently found between adjacent toes) stay moist, keeping the surrounding skin soft. The corn's center is not soft, however, but indurated. Although corns and calluses are often talked about together, they are separate conditions 9.
Corns generally occur on the tops and sides of the toes. A hard corn is a small patch of thickened, dead skin with a small plug of skin in the center. A soft corn has a much thinner surface, appears whitish and rubbery, and usually occurs between the toes. Seed corns are clusters of tiny corns that can be very tender if they are on a weight-bearing part of the foot. Seed corns tend to occur on the bottom of the feet, and some doctors believe this condition is caused by blocked sweat ducts 10.
Calluses are hard and rough-feeling areas of skin that can develop on hands, feet or anywhere there is repeated friction - even on a violinist's chin. Like corns, calluses have several variants. The common callus usually occurs when there has been a lot of rubbing against the hands or feet. A plantar callus is found on the bottom of the foot. Diagnosis and workup to exclude other differential diagnoses, a skin biopsy may be taken. Imaging studies can be used to detect any underlying bony abnormalities that cause abnormal pressure on the overlying skin. For this purpose, a plain radiograph usually suffices, but, occasionally, CT scanning is used 11.
Treatment: Treatment of corns include paring of the lesions, which immediately reduces pain. However, if an abnormal pressure source remains, the corn generally returns. If the source of any abnormal pressure is detected, this may be avoided, such as with orthotics and conservative footwear with extra toe space. If no other treatment is effective, surgery may be performed. Most corns and calluses gradually disappear when the friction or pressure stops, although your doctor may shave the top of a callus to reduce the thickness. Properly positioned moleskin pads can help relieve pressure on a corn. There are also special corn and callus removal liquids and plasters, usually containing salicylic acid, but these are not suitable for everyone.
Oral antibiotics generally clear up infected corns, but pus may have to be drained through a small incision. Creams may help soften the skin and remove cracked calluses. Apply the moisturizing cream to the callus, and cover the area for 30 - 60 minutes with a plastic bag or a sock - but only if instructed to do so by your doctor or podiatrist. Then gently rub off as much of the callus as you can with a coarse towel or soft brush. Using a pumice stone first to rub off the dead skin from a callus after a bath or shower and then applying moisturizing cream can also be effective. There are also stronger creams containing urea that might be more effective but do not use these unless recommended by your doctor or podiatrist. Do not use hydrocortisone creams, which only help with rashes and itching and are not needed for calluses. Moisturising your skin incorrectly can aggravate a fungal condition and should be avoided - especially moisturizing between the toes. You may consider surgery to remove a plantar callus, but there are no guarantees that the callus will not come back. A conservative approach is best initially. Keep your feet dry and friction-free. Wear properly fitted shoes and cotton socks, rather than wool or synthetic fibers that might irritate the skin. If a podiatrist (a foot specialist) or orthopedic specialist (a bone and joint specialist) thinks your corn or callus is caused by abnormal foot structure, your walking motion or hip rotation, orthopedic shoe inserts or surgery to correct foot deformities may help correct the problem 12.
TABLE 1: CLASSIFICATION OF CORN AND CALLUS13
| Grade | Description |
| 0 | No lesion present |
| 1 | No specific callus plaque, but diffused or pinched callus tissue present or in narrow bands |
| 2 | Circumscribed, punctuate oval or circular, well-defined thickening of keratinized tissues |
| 3 | Corn seed (heloma millare) or hard corn (heloma durum) with no associate callus tissues |
| 4 | Well defined callus plaque with definite corn within the lesion |
| 5 | Extravasations maceration and early breakdown of the structure under the callus layer |
| 6 | A complete breakdown of the structure of hyperkeratosis tissues, epidermis, extending to superficial dermal involvement |
FIG. 1: DIFFERENCE BETWEEN CORN AND CALLUS
Corns: A corn is a circumscribed hyperkeratotic lesion with a central conical core of keratin that causes pain and inflammation. The core in com which thickening of the stratum corneum, is a protective response to the mechanical trauma. This central core distinguishes the corn from callus. Difference between corns and callus Corns are smaller than calluses and have a hard center surrounded by inflamed skin. They develop on parts of the body that do not carry any weight, such as tops and sides of your toes. If corns are pushed, then they can cause pain or suffer from a dull ache. Calluses usually develop on the soles of the feet, especially under the heels or balls, on the palms, or the knees They are rarely painful and vary in size and shape. They can be more than inch in diameter, making them larger than corns.
Corns are divided into two subtypes:
- The hard corn (Heloma durum)
- The soft corn (Heloma molle)
Hard corn, which is the most common type, appears as a dry horny mass of hyperkeratosis with a hard central core. Hard corn most commonly occurs on the dorsolateral aspect of the fifth toe or the dorsum of the interphalangeal joints of the lesser toes.
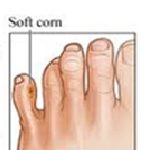
Soft corn results from the absorption of an extreme amount of moisture from perspiration and is noted by its characteristic macerated appearance. The soft corn is an extremely painful lesion that can be developed between the fourth and fifth toes. The common causes of hard and soft com are hammering toe deformity appearance 16.
FIG. 2: HARD CORN
FIG. 3: SOFT CORN
Etiology: Corns forms due to a combination of friction and pressure against one of the bony prominences of the feet. Inappropriate foot ware is frequently the cause - continue pressure and friction result in hyperkeratotic (excessive skin growth of keratinized layer) leaving even less space between the shoe and foot and therefore the corn is pressed unevenly more firmly against the underlying soft tissue and bone.
Signs and Symptoms for Corn on Foot: You have a corn or callus if you notice: 1. A thick, rough area of skin 2. A hardened, raised bump 3. Tenderness or pain under your skin 4. Flaxy, dry or waxy skin.
Pathogenesis prolonged mechanical stresses during weight bearing are thought to damage skin cells, which releases epithelial growth factors- increased keratinization results with increased bulk of stratum corneum. The rapid rate of epithelial transit is insufficient time for keratinocytes to mature and histologically, callus and com shows several changes from normal. Presence of nucleus within the keratin squames indicate incomplete keratinization know as porokeratosis. There is marked thickening of stratum corneum, and the granular layer becomes disrupted in callus and in corns it disappears completely. The dermal papillae and epid become flattened with those around becoming more elongated. The basal cell exhibit slight hyperplasia Corns shows additional differences in the ultrastructure of the cells, e.g. keratin fibril formation.
In the epidermis angiogenesis is present; otherwise, there are no signs of an inflammatory process. It is thought the changes relate to local biochemical reaction activated by the release of growth factor. Glycoprotein such as chalone for example, has been found in the Stratum germinitivum and Stratum spinosum. Chalones are tissue-specific and thought to control cell mitosis of epithelium, High concentrations of chalone result in low mitotic rate and slow keratinization and vice-versa. This could explain why some people produce more callus than others, i.e. they have present a low concentration of glycoprotein growth factor. Corns appear to have concentrated mass, which is usually referred to as “nucleus.” This gives the wrong impression of the genesis of the hyperkeratosis, as the skin does not grow from the nucleus but instead, the deeper segment represents the site of the epidermis, which offers the greatest resistance, from the complex, resultant, twisting forces acting intermittently and externally over the area of corn. Final resistance is offered by the hard structure beneath.
It is assumed the maceration, which appears as a milky yellow region under the callus plaque, is caused by trapped water within the side salt linkage of the Keratin molecules. This is thought to be a natural means of floating the heavy mass above. The lesion may be complicated by aseptic and infected inflammation. Springette outline model for the callus formation is shown in the table. Pressure on the cutaneous nerve ending with releases of prostaglandin as the part of acute inflammatory response occunts for sensitization and resultant felling of pain. This is enhanced with the presence of acute inflammatory response. Presence of prolong trauma will result in dermal changes starting with dermal protrusion of vascular and neural elements. Chronic inflammation caused by sharing results in deeper fibrosis, which anchors the lesion to the bone beneath; or alternatively, the development of sacs of fluid such as the pseudobursitis 17.
Callus: A clavus is a thickening of the skin due to intermittent pressure and frictional forces. These forces result in hyperkeratosis, clinically and histologically. The extensive thickening of the skin in a clavus may result in chronic pain, particularly in the forefoot; in certain situations, this thickening may result in ulcer formation. The word clavus has many synonyms and innumerable vernacular terms, some of which are listed in the Table below; these terms describe the related activities that have induced clavus formation.
Synonyms for clavus include callosity, a hyperkeratotic response to trauma; corn, heloma, or a circumscribed hyperkeratotic lesion that may be hard (i.e. heloma durum) or soft (i.e. heloma molle); and callous, callus, or a diffusely hyperkeratotic lesion. Localized callosities of the soles, which do not resolve, are termed plantar callus, heloma, tyloma, keratoma, or plantar corn. When callosities occur over 1 or more lateral metatarsals, they are termed intractable plantar keratoses.
Clinically, all these lesions look like hyperkeratotic or thickened skin. Maceration and secondary fungal or bacterial infections are a common overlying feature in heloma molle and diabetes. Plantar helomas tend to have a central keratin plug, which, when pared, reveal a clear, firm, central core. The most common sites for clavus formation are the feet, specifically the dorsolateral aspect of the fifth toe for heloma durum, in the fourth interdigital web of the foot for heloma molle, and under the metatarsal heads for calluses.
Pathophysiology: The shape of the hands and feet are important in clavus formation. Specifically, the bony prominences of the metacarpophalangeal and metatarsophalangeal joints often are shaped in such a way as to induce overlying skin friction. As clavus formation ensues, friction against the footwear is likely to perpetuate hyperkeratosis. Toe deformity, including contractures and claw, hammer, and mallet-shaped toes, may contribute to pathogenesis. Bunionettes, i.e., callosities over the lateral fifth metatarsal head, may be associated with neuritic symptoms due to compression of the underlying lateral digital nerves. Furthermore, Morton toe, in which the second toe is longer than the first toe, occurs in 25% of the population; this may be one of the most important pathogenic factors in a callus of the common second metatarsal head, i.e., an intractable plantar keratosis. The chronic or repetitive motion may also induce clavus formation, as is seen in computer users and text messengers (i.e., "mousing" callus). Callosities can also form from excessive leg crossing.
Medical Care: Treatment of a clavus should be aimed at reducing symptoms such as pain and discomfort with walking. The paring of the lesions immediately reduces pain. Once the etiology of the foot pressure irregularity is determined, attempts at pressure redistribution should be made. The use of orthotics and conservative footwear with extra toe space are often beneficial. When all else fails, surgery may be performed. If abnormal dermatoglyphics or pinpoint bleeding is seen, wart therapy is initiated. If normal dermatoglyphics are noted, salicylic acid compounds and orthotics may be beneficial. Relief of symptoms may be achieved by thinning and cushioning of the involved lesions. The paring of the lesions immediately relieves pain, especially with helomas.
Lesions may be maintained in this state if the patient uses short soaks and pumice stone debridement at home. Debridement may be enhanced with the use of keratolytic agents, such as ureas, alpha-hydroxy acid (e.g., glycolic, malic, or lactic acid), or beta-hydroxy acid (e.g. salicylic acid). Garlic extracts have also been described as being helpful. Self-adhesive pads are most effective for reducing thick lesions, whereas lotions, creams, and medicaments in petrolatum are best for maintenance.
Plants Profile: 31, 32, 33, 34
Lantana camara:
FIG. 4: LANTANA CAMARA
Biological Source: It is dried leaves of plant Lantana camara Linn. belonging to the family Verbenaceae. Lantana camara, is a species of flowering plant within the verbena family, Verbenaceae.
Synonym: Big-sage (Malaysia), wild-sage, red-sage, white sage Caribbean) (South Africa).
Description: Lantana camara has small tubular shaped flowers which each have four petals and are arranged in clusters in terminal areas stems. Flowers come in many different colors including red, yellow, white, pink and orange which differ depending on location in inflorescences, age, and maturity. After pollination occurs the color of the flowers change (typically from yellow to oranges, pinkish, or reddish), this is believed to be a signal to pollinators that the pre-change color contains a reward as well as being sexually viable, thus increasing pollination efficiency. The leaves are broadly ovate, opposite, and simple and have a strong odor when crushed. The fruit of L. camara is a berry-like drupe which turns from green to dark purple when mature.
Parts Used: Flowers and leaves
Distribution: Throughout India.
Chemical Constituents: Flavonoid, glycoside, polysaccharide, monosaccharide, alkaloids, steroids. It also contains terpenes and saponin responsible for wound healing activity uses. The essential oil, obtained by hydrodistillation of shade-dried leaves of L. camara, trans-caryophyllene (13.95%), bicyclogermacrene (9.77%), α-curcumene (8.57%) and D (3.13%) as the most abundant compounds. Monoterpene hydrocarbons, the second major class of compounds constituted 34.14% of the oil with sabinene (8.28%), α-pinene (4.03%) and γ-terpinene (3.83%) as the major components, whereas oxygenated monoterpenes comprised only 18.82%, having (E)-citral (6.90%), (Z)-citral (3.48%) and 1, 8 cineole (5.06%) in appreciable amounts. The remaining chemical constituents were detected in lesser amounts.
Uses: Studies conducted in that Lantana leaves can display antimicrobial, fungicidal and insecticidal properties. Use as antiseptic, inflammatory and antibacterial and also practically recovered cut, ulcers and swellings. Oleanolic acid is a chemical component consist of the root of this plant used as oral drugs that can cure human liver disorders such as anti hyperlipidemias and anti-tumor-promoting agent. The highest percentage of insecticide component in flower help the flower essential oil promotes the Aedes mosquito oviposition. Wound healing activity, anti-inflammatory activity, Lantana camara has also been used in traditional herbal medicines for treating various ailments, including cancer, skin itches, leprosy, rabies, chickenpox, measles, asthma. Lantana camara L. used in herbal medicine for the treatment of skin itches, as an antiseptic for wounds, and externally for leprosy and scabies. Major natural products investigated in Lantana camara L. belong to the group of triterpenoids.
Moringa oleifera: 32
Biological Source: Moringa oleifera is the most widely cultivated species of the genus Moringa, which is the only genus in the family Moringaceae.
Synonym: English common names include: Moringa, Drumstick tree, Dorseradish tree, Shevga.
FIG. 5: MORINGA OLEIFERA
Description: M. oleifera is a fast-growing, deciduous tree. It can reach a height of 10-12 m (32-40 ft) and the trunk can reach a diameter of 45 cm (1.5 ft). The bark has a whitish-grey color and is surrounded by thick cork. Young shoots have purplish or greenish-white, hairy bark. The tree has an open crown of drooping, fragile branches and the leaves build up a feathery foliage of tripinnate leaves.
The flowers are fragrant and bisexual, surrounded by five unequal, thinly veined, yellowish-white petals. The flowers are about 1.0-1.5 cm (1/2") long and 2.0 cm (3/4") broad. They grow on slender, hairy stalks in spreading or drooping later flower clusters which have a length of 10-25 cm. Flowering begins within the first six months after planting. In seasonally cool regions, flowering only occurs once a year between April and June. In more constant seasonal temperatures and with constant rainfall, flowering can happen twice or even all year-round.
Parts Used: Flowers and leaves, flavonoids and other compounds.
Distribution: Throughout India.
Chemical Constituents: Moringa oleifera is a medicinal plant widely used in folkloric medicine of Africa and Asia for the treatment of ailments such as ulcer, wound, inflammation, heart problem, cancer, stroke, obesity, anemia, and liver damage. The chemical constituents of the methanolic extract of Moringa oleifera leaves and seeds were investigated using gas chromatography-mass spectrometry. Sixteen chemical constituents were identified in the leaf methanolic extract; they are 9-octadecenoic acid (20.89%), L-(+)-ascorbic acid- 2, 6- dihexadecanoate (19.66%), 14– methyl- 8-hexadecenal (8.11%), 4- hydroxyl- 4- methyl-2-pentanone (7.01%), 3- ethyl- 2, 4-dimethyl-pentane (6.14%), phytol (4.24%), octadecamethyl-Cyclo-pentasiloxane (1.23%), 1, 2 benzene dicarboxylic acid (2.46%), 3, 4-epoxy-ethanone comprising (1.78%), N-(-1methylethyllidene)-benzene ethanamin main chemical components are pterygospermin, moringine, moringinine spirochin, behenic acid, moringic acid, niazinin A & B, niazimicin, campesterol, stigmasterol, beta-sitosterol and amino acids.
Uses: The root bark of the plant contains two alkaloids, viz. moringin, moringninie, and pterygospermin. It has anti-inflammatory antibacterial and counter-irritant action, which helps in wound healing. The leaves of the plant have also been reported for its antitumor, hypotensive, and antioxidant, radioprotective, anti-inflammatory and diuretic properties. It is mainly used for the bowel disorders, including arthritis, atherosclerosis, bladder infections, boils, burns, cancer, chronic fatigue syndrome, circulatory weakness, cold, congestion, constipation, diabetes, eye inflammations, fever, fractures, gastric ulcers, gingivitis, headaches, heart diseases, hypertension, immune weakness, indigestion, intestinal parasites, kidney disease, malaria, menstrual cramps, mouth sores, respiratory disorders, ringworms, sinusitis, sprains, stroke, skin inflammation and wounds.
The aqueous extract was studied and it was found that there was a significant increase in wound closure rate, skin breaking strength, granuloma breaking strength, hydroxyproline content, granuloma dry weight and decrease in scar area was observed.
Tecoma capensis: 33
Biological Source: It is a fresh leaf of plant Tecoma capensis Thunb. is a species of flowering plant in the family Bignoniaceae, native to Southern Africa. Despite its common name, it is not closely related to the true honeysuckle.
Synonyms: Bignonia capensis, Tecomaria capensis, and Tecoma petersii Cape honeysuckle.
FIG. 6: TECOMA CAPENSIS
Description: An erect, scrambling shrub, it grows to 2 - 3 m (7 - 10 ft) in height and a similar width. Normally evergreen, it may lose its leaves in colder climates. In certain habitats it may scramble, meaning that it shoots out long growth tips which lean on the stems and branches of other plants, as well as boulders, trellises, fences, and walls; this can lead to the plant appearing untidy. The leaves are up to 15 cm (6 in) long. They are opposite, slightly serrated, green to dark-green, and pinnate with 5 to 9 oblong leaflets.
The flowers are tubular, narrow, about 7.5 cm (3 in) long, and are produced at different times throughout the year. They are grouped in 10 - 15 cm (4 - 6 in) long terminal clusters. The flower color ranges from orange to orange-red to apricot.
Parts Used: Flowers and leaves.
Distribution: Throughout India.
Chemical Constituents: The Tecoma capensis, presence of sterols, flavonoids, terpenes, tannins, resins, carbohydrates and phenolic nucleus in all the species whereas, Phlorotannins and alkaloids remained absent in all the species. T. capensis and chloroform extract of T. rosea. Past studies proved that anti-dysenteric and anti-diarrhoeal properties of medicinal plants have been due to the presence of alkaloids, flavonoids, and saponins. Saponins were present in at least one extract of all tested flowers. Saponins have been responsible for antioxidant activities. Phenolic compounds, steroids, and glycosides were noticed in the tested flowers of Bignoniaceae. Tannins have been widely used in the treatment of sprains, bruises, and superficial wounds. Phytocompounds like flavonoids and phenolic compounds commonly found in plants have been reported to have multiple biological effects, including antioxidant activities.
Uses: The ethanolic extract of Tecomaria capensis was screened anti-inflammatory, antiulcer, analgesic activity. The plant is used as a traditional medicine to relieve pain and sleeplessness. Dried and powdered bark infusions are taken for sleeplessness. It is included in the list of African plants evaluated for in vitro antiplasmodial activity against Plasmodium falciparum. Previously methanol extract of Tecomaria capensis leaves reported as antimicrobial and antioxidant. Tecomaria capensis known to promote the wound healing process mainly due to their astringent, anti-microbial and free radical scavenging activities Tecomaria capensis significantly stimulated wound contraction. The breaking strength of the treated incision wounds increased in Tecomaria capensis extract when treated groups compared with the control group. These findings support the wound healing activity of this plant.
Barleria prionitis: 34
FIG. 7: BARLERIA PRIONITIS
Biological Source: It is a fresh leaf of plant Barleria prionitis, is a species of plants belonging to the family Acanthaceae.
Synonym: Barleria prionitis, Sanskrit kuranta; Marathi Vjradanti.
Parts of Plant Use: Leaves.
Distribution: Throughout India.
Description: Porcupine flower is an erect, prickly shrub, usually single-stemmed, growing to about 1.5 m tall. The stems and branches are stiff and smooth and light brown to light grey. The leaves are up to 100 mm long and 40 mm wide, and oval-shaped though narrow at both ends (ellipsoid). The base of the leaves is protected by three to five sharp, pale colored spines, 1020 mm long. The yellow-orange tubular flowers are found bunched tightly together at the top of the plant, but they also occur singly at the base of leaves. The flowers are 40 mm long and tubular, with several long protruding stamens. The seed capsule is oval-shaped and 13 - 20 mm long, with a sharp pointed beak. It contains two fairly large, flat seeds, typically 8 mm long by 5 mm wide, covered with matted hairs. Barleria has a central taproot, with lateral roots branching off in all direction.
Chemical Constituents: Barleria prionitis is often the host to larvae of the Phalanta phalantha and Junonia lemonias butterflies. Its leaves are known to contain 6-Hydroxyflavone, one of the chemical compounds that is a noncompetitive inhibitor of the protein cytochrome. From the aerial parts of Barleria prionitis, one new phenylethanoid glycoside, barlerinoside along with six known iridoid glycosides, shanzhiside methyl ester, 6-O-trans-p-coumaroyl- 8-O- acetylshanzhiside methyl ester, barlerin, acetylbarlerin, 7-methoxydi-derroside, and lupulinoside were isolated.
Uses: It has numerous medicinal properties including treating fever, respiratory diseases, toothache, joint pains and a variety of other ailments; and it has several cosmetic uses. A mouthwash made from root tissue is used to relieve toothache and treat bleeding gums.
For example, the leaves are used to promote healing of wounds and to relieve joint pains and toothache. Because of its antiseptic properties, extracts of the plant are incorporated into herbal cosmetics and hair products to promote skin and scalp health. Antioxidant activity reduces blood glucose level antiseptic.
Aim and Objectives: Aim of the present study is to develop an effective herbal formulation for the treatment of corn.
- To procure plants, Lantana camara, Moringa oleifera, Tecomaria capensis, Barleria prionitis.
- To collect and identify plants.
- To develop a formulation drug delivery system, g. gel, ointment.
- To evaluate formulation, g. gel, ointment.
Plan of Work:
Phase I: Literature survey selection of plants, collection of plant materials and its authentication
Phase II: Preliminary physicochemical and phytochemical screening, extraction/fractionation.
Phase III: Development of formulation, pharmaceutical evaluation of formulation.
Plant Collection, Authentification and Extraction:
- The leaves of plant Lantana camara, were collected from the local household garden of Amravati city.
- The leaves of plant Moringa oleifera, were collected from local household garden of Amravati city.
- The leaves of plant Tecomaria capensis were collected from Amravati local Area. The leaves Barleria prionitis were collected from V.M.V. College, Amravati.
- S. N. Malode, P.G. Department of Botany Government, Vidarbha Institute of Science and Humanities Amravati, have done authentification.
- Plant leaves drying and size reduction.
Extraction:
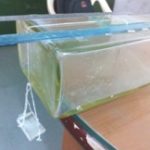
FIG. 8: WATER EXTRACTION
MATERIALS AND METHODS: Take Fresh leaves of plants, Lantana camara, Moringa oleifera, Tecomaria capensis, Barleria prionitis, reduction of size in equal parts. Take distilled water to add in to the RBF with raw material keep ready for aqueous extraction 100 gm material for 3 h process and then cool RBF filter it ready for formulation.
TABLE 2A: PRELIMINARY PHYTOCHEMICAL SCREENING OF WATER EXTRACT OF LANTANA CAMARA, MORINGA OLEIFERA, TECOMARIA CAPENSIS, BARLERIA PRIONITIS
| S. no. | Plants | LC | MO | TC | BP |
| Extract | Water | Water | Water | Water | |
| 1 | Carbohydrates | + | - | + | + |
| 2 | Protein | - | - | + | - |
| 3 | Flavonoids | + | + | - | + |
| 4 | Steroids | + | + | + | + |
| 5 | Alkaloids | + | - | + | - |
| 6 | Glycosides | + | + | - | - |
| 7 | Tannins | + | + | - | + |
| 8 | Resin | + | + | + | + |
LC: Lantana camara, MO: Moringa oleifera, TC: Tecomaria capensis, BP: Barleria prionitis
TABLE 2B: TEST FOR INORGANIC ELEMENTS
| S. no. | Test for Inorganic Elements | Inference |
| 1
2 3 4 5 6 7 8 9 10 11 12 |
Calcium
Magnesium Sodium Potassium Iron Sulphate Phosphate Chloride Carbonate Nitrates Zinc Aluminium |
-
+ - - + + - - + + + - |
(+Presence, -absence)
Development of Herbal Formulation: Ointments of various concentrations and combinations were prepared as below.
Plant water Extract: Lantana camara, Moringa oleifera, Tecomaria capensis, Barleria prionitis.
Excipients: Penetrating enhancer; alcohol, menthol.
Base: Emulsifying ointment (B.P. 1993) emulsifying wax hard paraffin, liquid paraffin.
Preservative: Propylparaben - Salicyclic acid-keratolytic agent Betamethasone - helps wound healing.
Formulation of Ointment: Weighed quantity of emulsifying ointment is taken in a tared vessel along with betamethasone salicylic acid and propylparaben and heated until the ointment melts. Extracts of plants Lantana camara (water extract), Moringa oleifera (water extract), Tecomaria capensis (water extract), Barleria prionitis (water extract) were dispersed in water in a separate container. The required quantity of menthol and alcohol is also added. This aqueous mixture is heated to the same temperature as that of emulsifying ointment. The aqueous phase is then added to the oily phase, in hot condition and the mixture is stirred until a cream consistency is obtained.
Evaluation of Formulation:
Physicochemical Parameters: All the formulation herbal ointment for corn caps were tested for the following parameters such as appearance, color, homogeneity, by usual inspections. The results are shown in Table 3. 35-48
Spreadability: 49
Method: Two glass slides of standard dimension (20 cm × 5 cm) were selected. The formulation was placed over one of the slides. The other slides were placed on the top of the ointment such that the formulation is sandwiched between the two slides in an area occupied by a distance of 6.0 cm, alongside 100 gm weight was placed uniformly to form a thin layer. The weight was removed, and the excess of ointment adhering to the slides was scrapped off. The two slides in position were fixed to a stand (45° angle) without slightest disturbance and in such a way that only the lower slides was held firmly by the opposite fangs of the clamps allowing the upper slides to slip off freely by the force of weight tied to it. 20 grams of weight was tied to the upper slide carefully. The time taken for the upper slide to travel the distance of 5 cm and separate away from the lower slides under the direction of weight was noted. The experiment of repeated and the mean time taken for three such dimensions was calculated. The results were recorded.
FIG. 9: SPREADABILITY APPARATUS
The spreadability is calculated by using formula
S = M × L / T
Where S = Spreadability, L = Length of glass slide, M = Weight tied to upper slide, T = time
Test for Thermal Stability: 49 In this test the oil separation from the ointment were tested at 60- 70% RH and 37 ± 1 °C in the humidity chamber.
Procedure: In this, a 20 mm broad and 5 mm stripe of ointment was spread on the internal wall of the beaker of 100 ml capacity, in its total heights. Kept the beaker for 8 h in the humidity chamber at 60-70 % RH and temperature of 37 ± 1°C. To pass the test, there should not be any oil separation in the cream. The results are shown in Table 8.
Determination of pH: 49 Hair dye might have a wide variety of pH mostly ranging from 5-9. The ointment, in general, has a pH between 6-9. Hazelton reported that there is little correlation between pH and irritancy. Harry’s pointed out that it may be difficult to obtain accurate pH reading even with a glass electrode. The electrode must be washed free from any residue of acid and alkali to ensure accurate reading.
Apparatus Used: pH meter (digital model -111E).
Test Procedure: All the formulations under test were oil in water semisolid emulsions. As pH of the creams not to be directly measured, here 10% dilutions were made were with distilled water and the resulting pH mixture was determined with a pH meter. The results are shown in Table 5.
Determination of Total Fatty Substance: 50-54
Principle of the Method: The emulsion is broken with dilute mineral acid and the fatty matter was extracted with petroleum ether. It is weighted after removal of the solvent.
Regents: Dilute hydrochloric acid - 1:1 (%) ethyl ether. Methyl orange indicator solution - dissolve 0 - l gm of methyl orange in 100 ml water. Sodium sulphate I desiccated,
Procedure: 2 gm of accurately weighted material was taken into conical flask, then 25 ml of dilute hydrochloric acid was added, and the flask was fitted into reflux condenser, it was boiled until the oil and water phases are separated Then contents of the flask were poured into 300 ml separating funnel and allowed cool to 20 °C. The conical flask was rinsed with 50 ml of diethyl ether in portion °M 0 ml. Then poured into separating funnel, the funnel was shaken and left separating the layers. The aqueous phase was separated and shaken with N portion of ether twice.
Then it was combined and washed them with H & r until free of acids (when tested with methyl orange indicator solution). Ether extracts were filtered through a filter paper containing sodium sulfate t0 conical flask which was previously dried at a temperature of 60 ± 2°C and weighed. The sodium sulfate was washed on filter paper with ether, and the washing was combined with the filtrate. The ether was distilled, and the remaining material in the flask was dried at a temperature of 60 ± 2 °C to constant mass. Calculation:
Total fatty substance, % by mass = 100 × M1
Where, M1 = Mass in gm of the residue and M2 = Mass in gm of the material taken for the test.
The results are shown in Table 9.
Test for Rancidity: This test was performed by using the phloroglucinol solution. The rancidity is due to the oxidation of the fats and oils; during oxidation free fatty acids are liberated. These free fatty acids react with the phloroglucinol of I solution and give pink color. This indicates the rancidity of the product. Procedure 10 ml of melted ointment was taken then added 10ml of concentrated I hydrochloric acid and 10 ml of phloroglucinol solution and shaken for one minute. The material should be taken to have passed the test if no pink color developed. The results are shown in Table 6.
Determination of Viscosity: Viscosity is the most important parameter in the evaluation of the I ointment. Viscosity governs the many properties of the product such as K spreadability, pourability of the product from the container, etc. As the viscosity, I is affected by many factors such as a change in temperature, manufacturing 1 condition, quality of raw materials, etc. It is very important to measure the I viscosity of the cosmetic product. Viscosity was measured by Brookfield H viscometer.
Procedure: The correct spindle was selected (spindle No. 4) for the given product I the operating condition was set up. Then the viscosity was measured directly at 30-rpm speed by keeping the torque constant. The mean was obtained. (By using Brookfield viscometer). The results are shown in Table 7.
Stability Study: 34, 35, 36 Stability may be defined as the ability of the drug to retain its properties within specified limits throughout its shelf-life improper storage of cosmetic product can lead to their physical deterioration and chemical degradation resulting in reduced activity and occasionally leads to the formation of a toxic degradation product. So stability studies are carried out for each product.The present stability studies are carried out according to lines given by International Council of harmonization (ICH guidelines) accelerated stability testing particular temperature is obtained a plot of 108 k versus l/t gives the straight line from which the value of rate and constant at room temperature (25 °C) is determined by extrapolation. Once K value is determined it can be used to estimate the time (shelf life) for 10% degradation (t 10%) at 25 °C with the help of the following equation for the first-order reaction. Ti0 = 0.104/k25
Procedure: The formulated ointment were kept for accelerated stability studies to observe the effect of temperature on pH (digital pH meter) and viscosity (Brookfield viscometer, by using spindle no. 4 and at 30rpm speed) of the creams. The formulations were kept at 4 °C, room temperature and 45 °C for one month. After every ten days, they were tested for pH, viscosity, and effect of color on hair strands. The results are shown in Table 10.
RESULTS AND DISCUSSION:
TABLE 3: PHYSICOCHEMICAL PARAMETERS
| Formulation | Appearance | Colour | Homogeneity |
| 1 | Cream like | Brown | Homogeneous |
| 2 | Cream like | Brown | Homogeneous |
| 3 | Cream like | Light Brown | Homogeneous |
TABLE 4: DETERMINATION OF SPREADABILITY
| Formulations | Time in sec | Mean
Time |
Spreadability
gm, cm/sec |
||
| I | II | III | |||
| Formulation 1 | 8 | 8 | 8 | 08 | 12.5 |
| Formulation 2 | 10 | 9 | 9 | 9.33 | 10.75 |
| Formulation 3 | 10 | 9 | 8 | 09 | 11.11 |
TABLE 5: DETERMINATION OF pH
| S. no | Formulations | pH |
| 1 | I | 5.8 |
| 2 | II | 6.9 |
| 3 | III | 6.5 |
TABLE 6: TEST FOR RANCIDITY
| Formulations | Results |
| I | No Rancid |
| II | Rancid |
| III | No Rancid |
| IV | No Rancid |
TABLE 7: DETERMINATION OF VISCOSITY
| S. no. | Formulations | Viscosity (Centipoise) |
| 1 | I | 7000 |
| 2 | II | 6400 |
| 3 | III | 8200 |
TABLE 8: THERMAL STABILITY
| S. no. | Formulations | Results |
| 1 | I | No Separation |
| 2 | II | No Separation |
| 3 | III | Slight separation |
TABLE 9: DETERMINATION OF TOTAL FATTY MATERIAL
| S. no. | Formulations | % Fatty Content |
| 1 | Formulation I | 10% |
| 2 | Formulation II | 10.5% |
| 3 | Formulation III | 12.5% |
Stability Study:
Effect of Temperature on the Viscosity (cps):
TABLE 10: FORMULATION 1
| Days | Temperature (ºC) | ||
| 4 ºC | Room Temperature (25 ± 2 °C ) | 45 ºC | |
| 0 | 6000 | 6000 | 6000cps |
| 10 | 6000 | 5800 | 5800cps |
| 20 | 5800 | 5800 | 5600cps |
| 30 | 5800 | 5600 | 5400cps |
TABLE 11: FORMULATION 2
| Days | Temperature (ºC) | ||
| 4 ºC | Room Temperature (25 ± 2 °C ) | 45 ºC | |
| 0 | 7400 | 7400 | 7400cps |
| 10 | 7200 | 7200 | 7200cps |
| 20 | 7000 | 6800 | 6600cps |
| 30 | 7000 | 6400 | 6400cps |
TABLE 12: FORMULATION 3
| Days | Temperature (ºC) | ||
| 4 ºC | Room Temperature (25 ± 2 °C ) | 45 ºC | |
| 0 | 8400 | 8200 | 8200cps |
| 10 | 8200 | 8000 | 7800cps |
| 20 | 7800 | 7400 | 7400cps |
| 30 | 7600 | 7000 | 7000cps |
SUMMARY AND CONCLUSION: Corn and associated risk is a very common skin problem among worldwide population very few formulations are available in the market. The present research is undertaken to develop corn treating formulation by using natural keratolytic property having plant parts. Selected plant collected from local Amravati region, identified and authenticated from a competent botanist. Preliminary Phytochemical screening showed the presence of keratolytic phytochemical like alkaloids steroids, tannins. Aqueous extracts were prepared for each plant part, four different batches of ointments with varying composition of plant extracts and other necessary ingredients. Ointment form of delivery preferred due to long term contact with corn and water resistant capacity. Developed batches evaluated for various pharmaceutical parameters like physicochemical parameters, phytochemical study, spreadability, total fatty substances, test for rancidity, test for thermal stability, determination of pH, determination of viscosity, stability study, subjective property. It is observed that F-III showed promising results in the pharmaceutical evaluation. Finally, it is concluded that F-III ointment comprising Lantana camara (5%) Moringa oleifera (5%) Tecomaria capensis (5%) Barleria prionitis (5%) will be useful herbal.
ACKNOWLEDGEMENT: Nil
CONFLICT OF INTEREST: Nil
REFERENCES:
- Calapai G: Drug Safety European legislation on herbal medicines: A look into the future 2008; 31: 428-31.
- Chan MFE, Mok YS, Wong STF, Tong FMC, Day CCK, Tang K, Wong DHH: Attitudes of Hong Kong Chinese to traditional Chinese medicine and Western medicine: Survey and cluster analysis. Complement Ther Med 2003; 11(2): 103-9.
- PM, Bloom B and Nahin R: Complementary and alternative medicine use among adults and children: the United StatesCDC National Health Statistics Report 2007: 12.access.
- KB and Ames BN: The free radical theory of aging matures. Physiol Rev 1998; 78: 47-81.
- Benzie IFF and Wachtel-Galor S: Biomarkers in long-term vegetarian diets. Adv Clin Chem 2009; 47: 170-208.
- Bozzetti F: Nutritional issues in the care of the elderly patient. Crit Rev Oncol Hematol 2003; 48: 113-21.
- Basra MK and Shahrukh M: Burden of skin diseases. Expert Rev Pharmacoecon Outcomes Res 2009; 271-83. doi: 10.1586/erp.09.23
- Denise B and Freeman DPM: Corns and Calluses Resulting from Mechanical Hyperkeratosis Am Fam Physician 2002; 65(11): 2277-2280.
- Richards RN: Calluses, corns, and shoes. Semin Dermatol 1991; 10: 112-4.
- Gu SX, Zhang AL, Coyle ME, Mo X, Lenon GB, Cranswick NE, Chen D and Xue CC: Chinese herbal medicine granules (PTQX) for children with moderate to severe atopic eczema: study protocol for a randomised controlled trial.
- Singh D, Bentley G and Trevino SG: Callosities, corns, and calluses. BMJ 1996; 312(7043): 1403-6.
- Murphy GA: Lesser Toe Abnormalities: Corns (Helomata and Clavi). In: Canale ST, ed. Canale: Campbell's Operative Orthopaedics. 10th. St. Louis, Mo: Mosby 2003; 4063-5.
- Martin JS, Hylton BM and Stephen RL: Distribution and correlates of plantar hyperkeratotic lesions in older people. Journal of Foot and Ankle Research Mulation for Treatment of Corn 2009; 2: 8.
- Freeman DB: Corns and calluses resulting from mechanical hyperkeratosis. Am Fam Physician 2002; 65(11): 2277-80.
- Ambikadattashashri K: Sushruta Samhita, with Hindi translation of the text. Varanasi: Chaukhamba Sanskrit Sansthan, Purvardha-Nidan Sthana, Chapter-13, Sloka-29, Reprint 2008; 30: 28.
- Murphy GA: Lesser Toe Abnormalities: Corns (Helomata and Clavi). Canale ST, ed. Canale: Campbell's Operative Orthopaedics. 10th. St. Louis, Mo: Mosby 2003; 4063-5.
- Singh D, Bentley G and Trevino SG: Callosities, corns, and calluses. BMJ 1996; 312(7043): 1403-9.
- DeLauro TM and DeLauro NM: Corns and Calluses. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ: Fitzpatrick's Dermatology in General Medicine. New York, NY: McGraw-Hill, Edition 7th, 2008; 97.
- Dehghani F, Merat A, Panjehshahin MR and Handjani F: Healing effect of garlic extract on warts and corns. Int J Dermatol 2005; 612-5.
- Mirakhmedov UM and Belova LV: Use of medicinal plants and preparations from them to treat various skin diseases. Vestn Dermatol Venerol 1983; 7: 23-7.
- Fedorov IP. Phytotherapy of common warts and dry corns. Med Sestra 1972(8): 48-9.
- Thomas EW: Corns and callosities. Practitioner 1947; 159(954): 487.
- Sadik F: OTC products for corns, calluses, warts. J Am Pharm Assoc 1970; 10(1): 8-12.
- Vijayshankar BV, Sharma M, Chandrashekar R and Manohar VR: A prospective study of prathisaraneeya apamarga kshara in comparison with prathisaraneeya palasha kshara in patients with charmakeela (warts) and kadara (corns). J Phyto 2014; 3(5): 330-336.
- Kanchan MB and Anantkumar V: Shekokar role of agnikarma therapy in the management of kadara (corn): A case report. Int J Ayur Pharma Research 2013; 1(3): 67-72.
- Jain VK, Ghindora GL, Paikra N and Dhirehe UK: Studies on surface tension of selected corns formulation by drop number method using Traube‟s Stalagmometer Technique.
- Carol J: Buck Compositions and methods for softening, thinning and removing hyperkeratotic tissue US 6858215 B2 [US patent] 28.
- Kiran P: Corns and Calluses: Overview of common keratotic lesions. US Pharm 2014; 39(6): 47-50.
- Nader P and Amir F: Dermatol Reports 2011; 3(1): e4.
- Ejaz S, Chekarova I and Cho JW: Effect of aged garlic extract on wound healing: a new frontier in wound management. Drug Chem Toxicol 2009; 32: 191-203.
- Nayak BS, Raju SS and Ramsubhag A: Investigation of wound healing activity of Lantana camara Sprague dawley rats using a burn wound model: International Journal of Applied Research in Natural Products 2008; 1(1): 15-19.
- Rathi BS, Bodhankar SL and Baheti AM: Evaluation of aqueous leaves extract of Moringa oleifera for wound healing in Albino rats. Indian Journal of Experimental Biology 2006; 44: 898-901.
- Saini NK, Singhal M and Srivastava B: Evaluation of wound healing activity of Tecomaria capensis Chinese Journal of Natural Medicines 2012; 10(2): 0138-0141.
- Patil SB, Naikwade NS, Kondawar MS, Magdum CS and Awalel VB: Traditional uses of plants for wound healing in the Sangli district, Maharashtra. International Journal of Pharm Tech Research 2009; 1(3): 876-878.
- Mukharjee PK: Quality control of herbal drugs. Business Horizons 2002; 357-360.
- Indian Pharmacopoeia. Govt of India, Ministry of Health and family welfare, published by the controller of publication, New Delhi 1996; 2(54): A-89.
- British Pharmacopoeia, Published on the recommendation of the medicines commission pursuant to the medicines Act - 1968, Department of Wealth and social security Home and health Dept. Ministry of Health and Social services for Northern Iceland 1988; 2: A-139 - A-140.
- Indian Herbal Pharmacopoeia: A Joint Publication of Regional Research Laboratory and manufactures Association 1999; 11 93-101.
- Kokate CK: Practical Pharmacognosy, Vallabh Prakashan, New Delhi, Edition 3rd, 1991; 107-111.
- Khandelwal KR: Practical Pharmacognosy, Techniques and experiment, Nirali Prakashan, Pune 149-156.
- Marie LL: A method for assessing occupational dermal exposure to ointment. Annual Occupational Hygiene 2004; 48(6): 553-559.
- Motoyoshi K: Enhanced comedo formation in rabbit ear skin by squalene and oleic perosice. British Journal of Dermatology 1983; 109: 191-198.
- Kulkarni GT and Suresh B: Stability testing of Pharmaceutical products: (A Overview). Indian Journal of Pharmaceutical Education 2004; 38(4).
- Walter YY: Accelerated temperature pharmaceuticals product stability determinations. Drug Development and Industrial Pharmacy 1990; 16(4): 551569.
- Wolfgang G: Stability testing in industry for Worldwide Marketing. Drug Development and Industrial Pharmacy 1988; 12(8/9): 1259- 1292.
- Khandelwal KR: Practical Pharmacognosy, Techniques and experiment, Nirali Prakashan, Pune 149-156.
- British Pharmacopoeia Published on the recommendation of the medicines commission pursuant to the medicines Act - 1968, Dept, of Wealth and social security Home and Health Dept. Ministry of Health and Social Services for Northern Iceland 1993; 2: A-139-A-140.
- Kokate CK: Practical Pharmacognosy, Vallabh Prakashan, Delhi, Edition 4th, 2001; 34.
- Sagarin B: Cosmetic science and technology. Edition 2nd, 321.
- Marie LL: A method for assessing occupational dermal exposure to permanent hair dye. Annual Occupational Hygiene 2004; 48(6): 553-559.
- Multimer MN, Riffskin C and Hill JA: J of American Pharmaceutical Association Sciences 1956; 45: 212.
- Michael J: Coughlin, from Oregon Health Sciences University, Portland, USA.
- Indian Pharmacopeia’s 1996; 2: A-53.
- Indian Pharmacopeia’s 1996; 2: A-157.
How to cite this article:
Thorat VH, Ghorpade SS and Patole T: Development and evaluation of polyherbal dermal formulation. Int J Pharmacognosy 2018; 5(4): 226-41. doi link: http://dx.doi.org/ 10.13040/ IJPSR.0975-8232.IJP.5(4).226-41.
This Journal licensed under a Creative Commons Attribution-Non-commercial-Share Alike 3.0 Unported License.
Article Information
6
226-241
746
1640
English
IJP
V. H. Thorat*, S. S. Ghorpade and T. Patole
Department of Pharmacognosy and Phytochemistry, SGB Amravati University, Amravati, Maharashtra, India.
vishalthorat15@gmail.com
23 November 2017
05 January 2018
13 February 2018
10.13040/IJPSR.0975-8232.IJP.5(4).226-41
01 April 2018